
Varicose Veins
- What are varicose veins?
- What causes varicose veins?
- How common are varicose veins?
- Can varicose veins cause symptoms?
- What should I do about my varicose veins?
- What happens when you see a vascular surgeon?
- Is treatment for my varicose veins essential?
- Can I live without my varicose veins?
- What treatment is available for varicose veins?
- Will treatment remove all of my varicose veins?
- Will my varicose veins come back after treatment?
- Varicose veins and pregnancy
- Useful links
- References
What are varicose veins?
Varicose veins are abnormally swollen (dilated) and tortous (twisted) veins. Varicose veins are usually situated quite near the surface and are often visible beneath the skin. Varicose veins can vary in size from quite small (2-3mm across) to very large (2-3cms across). Very small veins are called “thread veins” or “spider veins”. These veins are different to varicose veins because they are situated much closer or within the overlying skin. Although they may be unsightly, they are not the same as varicose veins and can be more difficult to treat. Reticular veins are obvious varicose veins which are present beneath the skin and easily visible, but rather smaller than the larger knobbly veins. Reticular veins may only bulge the skin slightly if at all, whereas varicose veins tend to produce marked bulging of the skin.
What causes varicose veins?
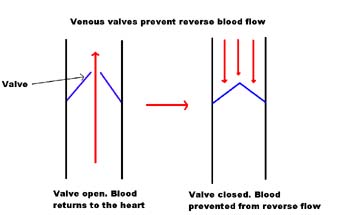
Veins are blood vessels that normally return blood from the leg upwards, back to the heart. Blood flow in the veins should also always travel from the superficial veins to the deeper veins in the legs. Blood will not normally travel downwards in the reverse direction or outwards from deep to superficial veins as there are one-way valves inside the veins that prevent this occurring (see opposite). In some people faults can develop in these valves (we do not know why for most), and blood is permitted to travel not only towards the heart, but can also travel backwards (reflux) towards the foot, especially on standing. Veins that reflux are said to be incompetent or to have incompetent valves. An artery is a different type of blood vessel which transports blood away from the heart, taking oxygen and nutrients to the tissues.
Because the valves in some veins are not working normally a higher pressure in the veins develops and they gradually become swollen and varicose, although this can take many years. Unfortunately, the faults in the valves cannot be cured. The clinical effects of varicose veins seem to be caused by prolonged high pressures in the veins and without abnormally high pressures symptoms or complications of varicose veins do not develop.
Risk factors for varicose veins include increasing age, a family history of varicose veins and obesity. Other associations such as with prolonged standing or pregnancy are not as clear cut. In some less common situations the causes for varicose veins are understood better. Occasionally direct trauma to the leg can lead to the development of a varicose vein. On other occasions patients may have had a deep venous thrombosis or DVT. If the blood clot that forms in the deep veins is not reabsorbed by the body then the only pathway for blood to drain from the leg is through the superficial veins which then enlarge to cope with the extra workload. To remove varicose veins in these circumstances would be potentially very dangerous as it would remove an important pathway for blood to drain from the leg back to the heart.
How common are varicose veins?
Varicose veins tend to become more common with increasing age. Thread veins are very common later in life and are a normal part of ageing. Eight out of ten people will develop thread veins.
Varicose veins usually run in the family and they may be made worse in certain circumstances such as pregnancy and obesity. One study (Cornu-Thenard, 1994) demonstrated that if both parents have varicose veins then the risk of their children developing varicose veins was about 90%. If one parent was affected by varicose veins the risk of men developing veins was 25% (1 in 4) and for women 62% (more than 1 in 2). About 20% (1 in 5) of patients presented with no history of veins in the parents. Large varicose veins may be more common in men. About 39% of men and 32% of women developed large varicose veins in the Edinburgh vein study (Evans CJ, Lee AJ, Ruckley CV, Fowkes FGR). It is commonly thought that varicose veins are more common in women, but this may not be the case, although many more women attend clinics to have their varicose veins assessed. There are many possible reasons for this imbalance. Men are notorious for not taking health issues seriously, although varicose veins can cause just as many problems as in women. Men also wear trousers and tend to have hairy legs which cover the varicose veins to some degree. In women varicose veins can be much more noticeable.
Varicose veins become more common with age and also seem to be more common in the Western world.
Can varicose veins cause symptoms?
Varicose veins are viewed in many quarters as a minor disorder with a low priority for treatment. However, they are common and do cause significant concern among patients. Varicose veins can cause no symptoms at all and will merely be a nuisance because of their unpleasant appearance. However, varicose veins can cause heaviness or tension in the legs. There is often a feeling of swelling, aching, restless legs, cramps and itching. Symptoms such as these are often worse after a long day of standing. Symptoms are often worse in hot weather or after exercise and many women find symptoms are worse during their periods. During pregnancy many women notice that their varicose veins become more prominent and more symptomatic. In many patients these problems will settle after the birth of the baby. Unfortunately, symptoms from varicose veins are rather non-specific and it is difficult to correlate the severity of symptoms with the severity of the venous disease, but venous disease has been shown to have significant effects on quality of life. In the worst case of venous ulceration the impariment in quality of life was comparable to patients with chronic lung and heart disease (Carradice et al 2011). It is also clear that symptoms do mainly resolve after varicose vein treatment.
Although most patients will not develop complications, varicose veins can sometimes cause more serious problems such as:
Superficial thrombophlebitis – this is an inflammation in the varicose veins. The superficial varicose veins become red, hot, tender and painful and blood clots form in the superficial veins. This can take many weeks to resolve. In patients with above knee phlebitis about 20% (1 in 5 patients) will have an underlying thrombosis in the deep veins (Deep Venous Thrombosis or DVT). Sometimes when a severe phlebitis has resolved the varicose veins may disappear, but it is important that you are assessed by a vascular surgeon to ensure there are no residual abnormalities that may require treatment to prevent further phlebitis.
Chronic venous insufficiency – the development of brown discolouration of the skin at the ankle (pigmentation), varicose eczema and thickening in the tissues around varicose veins (liposclerosis) are signs that more extensive tissue damage is occurring.
Varicose ulceration – if the tissue damage becomes great enough, ulcers can develop in the skin just above the ankle. Many patients are concerned when they hear the term ulceration, but it only means that there has been a loss of skin and that the tissues beneath the skin are exposed.
Bleeding – bleeding from varicose veins is relatively uncommon especially from the large bulbous type varicose veins. If bleeding does occur it tends to be from smaller very superficial venous blebs in the skin.
What should I do about my varicose veins?
If your varicose veins are causing you concern for any reason, then you should seek a medical opinion. If you wish to have treatment for your varicose veins, develop severe symptoms or more serious complications of varicose veins then it is essential you have a consultation with a vascular surgeon. A phlebologist is a doctor who also treats varicose veins. There are increasing numbers of doctors from many different specialties treating varicose veins. This is partially because of the availability of newer techniques which can be performed outside of an operating theatre setting, but it is also because there is a significant commercial element involved. It is very important that when you discuss treatments with your surgeon/phlebologist that you are happy with their level of experience in venous disease. The service provided should be comprehensive. From a detailed history, examination and ultrasound vein mapping to a capability to offer a range of treatments from surgery, ultrasound guided sclerotherapy, EVLT/RFA and microinjection sclerotherapy. If your doctor has only skills in one treatment then they are only likely to offer that one treatment. If your doctor has skills in all areas then it is more likely you will receive an unbiased assessment of the treatment that is likely to be most effective in your particular circumstances.
There is nothing that can be done to prevent varicose veins. It would be impossible to remain permanently off your feet, which is a good way to reduce the pressure in the veins. If you are on your feet the best thing to do is to keep moving, as walking tends to lower the pressure in the veins. Compression stockings can be very helpful in lessening symptoms and an improvement in symptoms when wearing stockings can be an indication that treatment for the veins will be helpful.
It is probably best to avoid using hot wax for hair removal on the legs if you have prominent veins.
What happens when you see a vascular surgeon?
When you consult a vascular surgeon a detailed history will be taken with regard to your varicose veins and the nature of your symptoms. An examination of the leg is performed to look at the distribution of the varicose veins and for signs of tissue damage secondary to the varicose veins. Your general health will also be assessed.
It is also important to undergo a detailed ultrasound mapping scan in order that your surgeon can plan the most effective treatment for you. This is particularly important if you have had previous surgery, a history of thrombosis in the veins, valve abnormalities behind the knee or leg ulceration. The scan is called a Colour Flow Duplex scan. It is now an essential pre-operative investigation in all patients with varicose veins. There is good evidence that results are better in patients who have had a preoperative scan (Blomgren et al, 2005). The scan will provide a map for the surgeon detailing the exact problems in the veins.
Is treatment for my varicose veins essential?
If you have developed complications of varicose veins then it is advisable to proceed with treatment. This will halt the process that has caused the complications and will give the best chance of reversing any changes that may have taken place in the skin or tissues of the leg.
In patients with simple varicose veins that have not caused serious complications, treatment can be considered optional. In other words the patient can make a decision to proceed with treatment if they wish, but it is not essential, as most patients with simple varicose veins will not develop serious problems. Most patients decide to proceed with treatment if the varicose veins are causing symptoms or the appearance is unsightly. The choice is yours in consultation with your surgeon after you have weighed up the problems the varicose veins are causing against the treatment recommended. There is no foolproof way to predict the risk of future problems from your veins if they have not already caused complications.
Can I live without my varicose veins?
Yes. For the vast majority of patients this will not be a concern. The veins that are being removed are not functioning normally in any case. A common question is whether removing varicose veins puts extra load on the remaining veins and hence a risk of recurrent veins. There is no question that if veins are removed then the same amount of blood will have to travel through a slightly reduced number of veins. This is not a significant issue because there is excess vein capacity in the legs with a considerable amount of redundancy built into the venous system. It is important to remember that the venous system of the leg has already changed to accommodate the altered flow and pressures in the abnormal veins.
There are some rare situations when varicose veins are present and the deep veins in the leg are blocked. This may make it unsafe to have superficial varicose veins removed. Your surgeon will have checked for this preoperatively. Some patients are concerned that they may need their veins for possible heart or leg bypass surgery later in life. In fact varicose veins are unsuitable for use in these situations. Varicose veins are diseased veins and would be detrimental to success in these operations, where more healthy veins are required. It is also relatively uncommon for patients who have their varicose veins removed to subsequently require bypass surgery.
What treatment is available for varicose veins?
To a large extent the treatment will depend on the sites of the major valve problems in the varicose veins, the distribution and tortuosity of the veins and the severity of the varicose veins.
Surgery – this is still the most common form of treatment for varicose veins and is a very effective way of completely removing veins.
RFA (RadioFrequency Ablation) – this is a newer method of treating the source of the varicose veins. It is a replacement for the stripping part of the operation but may need supplementary treatment either with injections or minor avulsions to the visible veins. There is reasonable evidence that RFA is superior to EVLT.
EVLT (Endovenous Laser Therapy) – this is a similar to RFA. It is also a replacement for the stripping part of the operation, but also may not deal with all of the visible varicose veins.
Injection sclerotherapy – this is used in all types of varicose veins and a microinjection technique may be used for thread veins. It does not seem as effective as other techniques for larger varicose veins.
Compression stockings – these may be all that is required if aching and swelling are the main problems. It is essential that the correct grade of stocking is used after proper fitting. Many patients find these very effective for symptoms although they may be inconvenient particularly in warm weather. For patients with simple varicose veins a Class I compression stocking is the appropriate grade to use. This is the lightest compression stocking, but will still feel quite firm and can be awkward to put on. Once the stockings are in place they are comfortable. If you have had problems with complications from your varicose veins then it may be more appropriate to use a Class 2 compression stocking which gives more support. Stockings are available in two main lengths – above the knee or below knee. Either type are suitable although some patients find the above knee stockings tend to roll down. Depending on the type of varicose veins a full length or below knee stocking may be most appropriate and this will also depend, to some extent, on the shape of your leg. There is a tight retaining band in below knee stockings which can compress and cause phlebitis in patients with varicose veins just below the knee. In these circumstances an above knee stocking may be better.
Will treatment remove all of my varicose veins?
Probably not. No treatment can erase every visible varicose vein, but most patients are satisfied with the vast improvement that can be gained by undergoing treatment. Your surgeon should indicate to you before treatment, where you will gain the most benefit and which varicose veins may be difficult to treat. It is more difficult to improve the appearance of spider veins. Some patients do notice that their spider veins become much less noticeable after surgery to remove the larger varicose veins which should always be treated first.
Will my varicose veins come back after treatment?
Varicose veins that have been physically removed cannot reappear, but there is no treatment available that does not have a risk of recurrent varicose veins. New varicose veins can sometimes appear even after satisfactory treatment. It is possible to remove existing varicose veins, but it is not possible to remove the tendency to develop varicose veins, whatever the treatment. Sometimes in patients who have had injection treatment the varicose veins that have been injected can reopen as they have not been physically removed.
Reflux (abnormal flow) in deep veins may be a cause of recurrent veins, but this is usually not treatable (Ali SM, Callam MJ, 2007).
Even if varicose veins do return it will usually take many years if the most appropriate and effective treatment has been performed.
Varicose veins and pregnancy
Many women find that during pregnancy, they can either develop varicose veins or pre-existing varicose veins can become larger or cause problems. There is no doubt that pregnancy does affect the veins in the legs, but pregnancy does not cause varicose veins, unless there is already an underlying tendency to develop them. If pregnancy did cause varicose veins they would be more common in women, but the Edinburgh vein study has shown that this is not the case.
It is not known exactly why the veins change during pregnancy, but there are a number of possible reasons. Firstly, the womb and the baby will press on veins in the pelvis causing obstruction to the return of blood to the heart. This obviously becomes worse as the pregnancy progresses and may lead to the veins in the leg becoming swollen and symptomatic. Hormones released by the body during pregnancy may also be a factor. The blood volume and the general effect of pregnancy on the blood circulation may also be important. Following pregnancy all these factors disappear and in many women so do problems with their varicose veins. Vulval varicosities are a particular problem in pregnancy but usually resolve after birth of the baby. It is uncommon to see persisting vulval varicosities outside of pregnancy. If varicose veins persist they should be treated if necessary.
There is no reason why women should wait to have their varicose veins treated until after they have completed their family. Existing varicose veins may cause problems in a subsequent pregnancy and the risk of developing further veins is not affected by whether surgery has been performed or not. If a young woman has symptomatic varicose veins that she wishes to be treated then this can proceed whether or not she will have a further pregnancy.
Useful links
http://www.nlm.nih.gov/medlineplus/varicoseveins.html – A service from the US National Library of Medicine and the National Institutes of Health in the USA with a series of links to sites with good information on various aspects of diagnosis and treatment of venous disease.
http://www.vdf.org/diseaseinfo/varicose/
http://www.vascularweb.org/vascularhealth/Pages/varicose-veins.aspx
http://www.nhs.uk/conditions/Varicose-veins/Pages/Whatarevaricoseveins.aspx
http://www.mayoclinic.com/health/varicose-veins/DS00256/DSECTION=1
http://www.gvg.org.uk/vvinfo.htm
References
Cornu-Thenard A, Boivin P, Baud J-M, De Vincenzi I, Carpentier PH. Importance of the familial factor in varicose disease. J Dermatol Surg Oncol 1994; 20: 318-326.
Evans CJ, Lee AJ, Ruckley CV, Fowkes FGR. How common is venous disease in the general population? in Venous Disease, p 3-14. Ruckley CV, Fowkes FGR, Bradbury AW (Eds), Springer 1998.
Carradice D, Mazzari FAK, Samuel N, Allgar V, Hatfield J, Chetter IC. Modelling the effect of venous disease on quality of life. Brit J Surg 2011;98:1089-1098 .
Blomgren L, Johansson G, Bergqvist D. Randomized clinical trial of routine preoperative duplex imaging before varicose vein surgery. Brit J Surg 2005; 92: 688-694.
Campbell B. Varicose veins and their management. BMJ 2006;333: 287-92.
Ali SM, Callam MJ. Results and significance of colour Dupex assessment of the deep venous system in recurrent varicose veins. Eur J Vasc Endovasc Surg 2007; 34: 97-101.