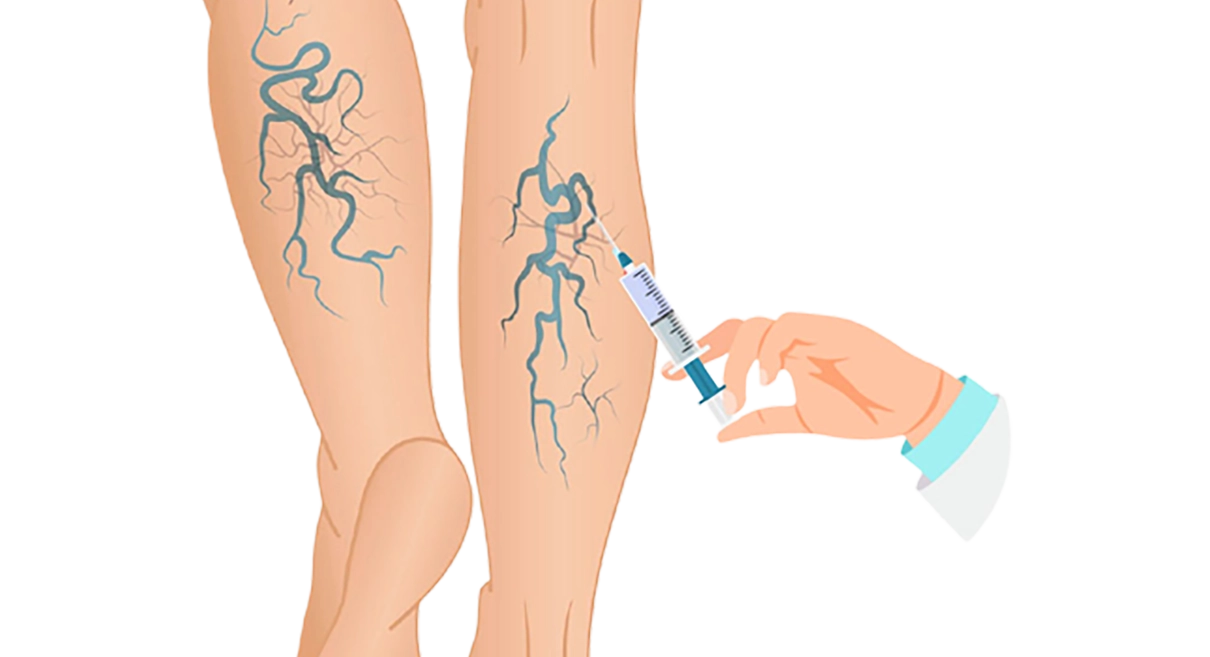
Sclerotherapy Treatment
for Varicose Veins
- What is vein injection sclerotherapy?
- Which varicose veins are suitable for injection sclerotherapy treatment?
- Before your vein injection sclerotherapy
- The technique of vein injection sclerotherapy
- After the vein injection sclerotherapy
- Ultrasound guided foam sclerotherapy (UGFS)
- Possible complications of injection sclerotherapy
- Useful links
- References
What is vein injection sclerotherapy?
Injection sclerotherapy is a treatment that intentionally damages the lining (endothelium) of veins by injecting a chemical into the vein and inducing a chemical phlebitis or inflammation. By doing this and then applying pressure the vein walls stick together. The vein can then no longer fill with blood and so it is obliterated. The compression applied after the injection is an essential part of the therapy. Sclerotherapy has been around in one form or another for well over 100 years and there are descriptions going back much further. It has risen and fallen in popularity as techniques have evolved.
Foam sclerotherapy is an evolution of earlier methods and uses a standard sclerosant such as STS (sodium tetradecyl sulphate) and mixes it with air or carbon dioxide in various ratios to create a foam. This foam is then injected into the veins. By using STS as a foam rather than a liquid the effect is potentiated especially in larger veins.
Ultrasound guided foam sclerotherapy is a further development in which the foam injection is guided by ultrasound. The ultrasound probe is able to track the needle entering the vein and ensure the injection takes place in the appropriate place. The dispersion of the foam can then tracked by ultrasound.
Microinjection sclerotherapy is used for very fine spider veins and uses a very fine needle.
Examples of sclerosants are STS (sodium tetradecyl sulphate), 20% hypertonic saline and polidocanol. STS and polidocanol can be used as a foam, but hypertonic saline can only be used as a liquid for fine thread veins. STS and polidocanol are the commonest sclerosants in current use.
Which varicose veins are suitable for injection sclerotherapy treatment?
There is a trend in recent years to less invasive treatments for varicose veins that enable a walk in-walk out service. The resurgence in injection sclerotherapy is part of that trend. Some practitioners will treat any patient with varicose veins by injection, but even amongst the sclerotherapists there is increasing recognition that major junctional reflux (see below) and particularly large veins are probably best treated by alternative means. Some practitioners will inject any abnormal vein and use sclerotherapy exclusively of any other treatment.
Major juntional reflux is present when the major valves at the groin (sapheno-femoral junction) or behind the knee (sapheno-popliteal junction) do not function normally. If there are problems at these locations your veins are best dealt with using other treatment methods for the majority of patients. Sclerotherapy works most effectively in smaller varicose veins or spider/thread veins. Sclerotherapy can be effective in any type of vein, but overall it tends to be less successful than other treatments with major varicose veins. For large varicose veins with faults in the valves at the groin there is probably a 15-20% chance of the injections not working with a single treatment (Rasmussen et al 2011) and sclerotherapy was the least successful treatment when compared with surgery, radiofrequency ablation and endovenous laser in this situation. Although it is possible to achieve improvement with these techniques, there is also a trade-off in terms of the time taken for vein resolution. A single treatment session is also unlikely to bring about the desired results. However in the right patients it can be very effective.
Deciding whether your veins are suitable for injection sclerotherapy requires experience, knowledge and practice with all modalities of treatment. It is also important to balance the potential risks and complications against any possible benefit. In patients with multiple coexisting medical problems it may well be more appropriate to avoid using surgical methods even in large veins.
Even if your veins are suitable for injection sclerotherapy, it is important that you have a frank discussion with your surgeon about the potential benefits and limitations of injections. It is important to be clear from the beginning what will be possible and what will not be possible. In some patients with very minor thread veins, injections may leave skin pigmentation that is no real improvement on the actual veins themselves. In these circumstances treatment will not improve the appearance of the veins and the use of false tan and camouflage cosmetics may be the best way to hide the visible veins.
Take care when reading advertisements offering injection treatments. Some of the claims are often misleading. ALL treatments have a failure rate and injection sclerotherapy is no exception. Injection sclerotherapy may appear to be a cheaper option if you are paying personally for the treatment, but this should not be the only consideration. In the long run expenses can be greater if a less effective or inappropriate treatment has been used.
Before your vein injection sclerotherapy
Well fitting compression stockings are an important part of the post injection regime and you should be measured up for these before the treatment session so they are available to put on immediately after your injections. There is a theoretical risk that taking the oral contraceptive pill or hormone replacement therapy at the time of your injection could increase the risk of a serious thrombosis. If they are stopped before your injection treatment, it is very important to think about other contraception methods.
It is important after the injections that you do not stand still for long periods. If you have a job that involves alot of standing it is important to arrange a few days off work after the injections or at least the ability to rest with your leg up when required. Avoid committments that force you to stand still for lengthy periods for the first few days after treatment.
The technique of vein injection sclerotherapy
The veins that may benefit from injections are identified. For spider veins I inject a small amount of liquid sclerosant into the visible veins usually at multiple sites. Many microinjections can be performed at a single sitting. Immediately after the injections the areas injected tended to become red and have a slightly inflamed appearance. This is not painless but the discomfort is minimal. The video below shows spider veins being injected.
For larger veins the STS liquid is made into a foam. The foam is created by mixing the STS with room air in a 1 to 4 ratio. Some practitioners use carbon dioxide. Before injecting I usually cannulate the veins to be treated. This involves placing a plastic tube or needle into the veins either under direct vision or sometimes using ultrasound guidance. The amount of treatment that can be administered at a single injection session will depend on the number and type of veins being treated and the amount and concentration of sclerosant being used. The injection is performed with the patient lying on a bed but with the leg elevated.
With liquid injections for spider veins using a low concentration of STS or polidocanol there is rarely an issue of exceeding the maximum dose. When injecting foam there are other concerns besides exceeding the maximum dose of STS. Foam contains thousands of tiny air bubbles which can be dangerous in excess. Most guidelines will recommend 10-15mls of foam as the maximum volume of foam that can be injected at any one sitting. This is because there is no way to contain the foam in the injected vein. Although most of the foam will remain in the vein some will always travel into the circulation even with the best attempts to prevent foam dispersal. As long as the volume is kept low this doesn’t appear to cause problems, but larger volumes may put patients at higher risk of complications (see below). There are practitioners that will inject 30-40 mls of foam at one sitting but I would not advise or perform this treatment.
After the vein injection sclerotherapy
After the injection a cotton wool pad is applied over the course of the injected veins followed by a stocking. After your injections you should go for a short walk of approximately 15 minutes. After that time you can carry on normal daily activities. Try to avoid standing still for long periods. If you are on your feet it is better to keep walking and if sitting to keep your legs elevated.
If wearing bandages, your surgeon will advise how long this is required. Stockings should be worn at all times day and night. Most surgeons would advise 14 days of compression for significant size veins. You can shower wearing the stockings and then use a hair dryer to dry the legs. Advice on the exact compression regime will vary and there is debate amongst practitioners on the appropriate level of compression as well as its duration.
The success of the injection treatment relies partly upon the pressure that the stockings apply to the injected area, in association with the damage caused by the sclerosant. It is important to take regular walking exercise after your treatment.
Ultrasound guided foam sclerotherapy (UGFS)
Ultrasound guided foam sclerotherapy is the latest development in the sclerotherapy field, despite being known about since 1939. The principle is the same as conventional sclerotherapy. The sclerosant is used to obliterate varicose veins.
The new points in this technique are that the liquid sclerosant is agitated to produce a foam-like mixture which is basically air that is mixed with sclerosant. This looks just like shaving foam. When this is injected into the veins it can be traced using an ultrasound scanner. Using ultrasound should improve accuracy and the use of foam appears to maximise the effect of the injection (Alos et al, 2006). Because a foam is required only sclerosing agents that can produce a foam can be used such as STS. In practice it is difficult to actually control the flow of foam and it aill always enter the main circulation to a greater or lesser degree. The safest technique appears to be to inject with the leg elevated and without pressure applied at the groin. There is also debate about whether it is safe to use air or whether other gases such as carbon dioxide should be used. Whether the gas injected should be sterile is also uncertain. Different types of syringe with differing silicone contents can affect the stability of the foam.
UGFS certainly can be effective initially (Darke SG, Baker SJA, 2006), but its medium to long term results are not reliably known. There are publications which claim effectiveness for the UGS technique, but frequently more than one session of injections are required for residual veins. It is also difficult, if not impossible, with UGS to perform a chemical sapheno-femoral ligation that is equivalent to the surgical treatment at this site. Ineffective treatment at this site is known to cause and to be a predictor for varicose vein recurrence. In fact for groin reflux in a trial comparing all the major treatments foam sclerotherapy came out as the least effective treatment with a 15-20% initial failure rate. There is also evidence that initial success for foam sclerotherapy may not be as durable as other treatments. This may at least partly be dependent on the size of the vein – larger veins being more difficult to treat.
Ultrasound guided foam sclerotherapy can be a very effective technique provided it is used appropriately. It is still not clear whether air or carbon dioxide gives better results. The exact ratio of air to liquid STS, optimal concentrations of STS foam for different veins and use of syringes with differing silicone contents can all influence foam production and stability but there is no first class evidence to favour one technique over another.
Possible complications of injection sclerotherapy
Sclerotherapy is not without potential complications. For the vast majority of patients sclerotherapy is very safe and most patients experience minimal discomfort, but it is not completely pain free and occasionally the thrombosed veins can be moderately uncomfortable. Following sclerotherapy for larger veins they become very hard and lumpy but this will gradually resolve and the veins disappear. Following microinjections the spider veins can initially look a little worse as congealed blood in the veins looks darker but this also will resolve. Over the first few weeks following the injection, any slight discomfort, hardness or tenderness at the injection site(s) should gradually subside. If there is excessive redness, swelling or tenderness, this means you should rest more, with the leg raised so that the heel is higher than the hip. If you are concerned see your surgeon.
Brown staining of the skin around the site of the injection and along the line of the treated vein is quite a common event. Most patients experience complete or near complete resolution but this can take up to 12 months after the injections.
A persistent hard “cord” in the line of the vein – this usually occurs after injecting bigger varicose veins and means a small amount of blood has clotted in the vein. It is not dangerous and will resolve.
Bruising – this is a common complication but will resolve completely often within one to two weeks.
Allergy – this is a rare complication. Allergy to sulphur containing antibiotics does not seem to present a risk of also having an allergy to STS.
Visual disturbance – this is a rare complication (about 1 in 100 or 1%) for patients undergoing foam sclerotherapy. Patients experience a sparkling appearance in their vision which resolves after about 15 minutes. One study reported this complication in up to 3% of patients.
Rare instances of transient stroke reported (Forlee MV et al 2006). This is thought to be due to the foam bubbles travelling in the blood vessels to the brain. This is more likely to happen in patients with an occult patent foramen ovale (PFO). An interesting study (Wright, 2010) examined how common PFO was in patients with significant truncal varicose veins. In the general population about 25-30% of patients are thought to have a PFO which doesn’t affect them in day to day life and they are usually unaware of its presence. In the study 58.8% of patients were found to have a PFO. In most patients undergoing foam sclerotherapy to major veins, foam bubbles can be seen travelling in the blood to the heart. For the majority of patients this does not appear to be a concern, but because of potential risks I prefer to reserve UGFS for patients without major junctional reflux and keep the volume injected to a minimum.
Slight blistering and occasionally ulceration of the skin at the injection site – this is rare but usually means the fluid has been injected around the vein rather than into the vein. It is much more likely to occur when using higher concentrations of sclerosant.
The injection may fail to obliterate the vein.
Deep venous thrombosis – although the risk of this is low it does occasionally occur. It may be related to the volume of sclerosant, particularly foam, that is injected. Larger volumes of foam injected close to the deeper veins may present more risk.
Useful links
http://www.dermnetnz.org/dna.cosderm/sclero.html – NZ dermatological society site with information on injection sclerotherapy
http://www.hta.ac.uk/fullmono/mon1013.pdf – Extensive review on surgical treatment and comparison with sclerotherapy.
http://besthealth.bmj.com/x/topic/392664/treatment-points.html
http://www.medi-data.co.uk/varicose-veins/threadveins.html
References
Alos J et al. Efficacy and safety of sclerotherapy using polidocanol foam: a controlled trial. Eur J Vasc Endovasc Surgery 2006; 31: 101-107.
Darke SG, Baker SJA. Ultrasound-guided foam sclerotherapy for the treatment of varicose veins. Brit J Surg 2006; 93: 969-74.
Forlee MV, Grouden M, Moore DJ, Shanik G. Stroke after varicose vein foam injection sclerotherapy. J Vasc Surg 2006; 43: 162-164.
Wright DD, Gibson KD, Barclay J, Razumovsky A, Rush J, McCollum CN. High prevalence of right-to-left shunt in patients with symptomatic great saphenous incompetence and varicose veins. J Vasc Surg 2010; 51: 104-7.
Rasmussen LH, Lawaetz M, Bjoern L, Vennits B, Blemings A, Eklof B.Randomized clinical trial comparing endovenous laser ablation, radiofrequency ablation, foam sclerotherapy and surgical stripping for great saphenous varicose veins. Brit J Surg 2011;98:1079-1087.