Atherosclerosis
Hardening of the Arteries
What is hardening of the arteries?
Hardening of the arteries (or atherosclerosis) is a degenerative disease of large and medium sized arteries. Inflammation seems to have an increasingly important role in the process, in which immune mechanisms interact with metabolic factors. This influences the initiation, propagation and activation of atherosclerotic lesions within the arteries (Hansson GK, 2005).
The intima (or innermost layer of the artery) becomes thickened by the development of fibrous tissue and the accumulation of lipid (fat). Although the arteries become progressively damaged over many years, the initial changes can occur in early adulthood (20-30yrs). Hardening of the arteries is not an inevitable result of ageing, but it is more common in the elderly.
The normal artery consists of three layers. The intima or inner layer is the surface in contact with flowing blood. A single layer of cells (endothelial cells) lines the whole of the arterial (and venous) system. It is a highly complex and important layer. It is these cells which interact with flowing blood. These cells are not simply a passive lining, but are crucial cells involved in wound healing, inflammation, blood clotting and immunity. These cells are supported by a matrix of thin tissue. Under this matrix is the middle layer (or media) consisting of muscle cells which can cause an artery to constrict or dilate. The outer layer (or adventitia) is mainly fibrous tissue. A normal artery is very soft, pliable and elastic.
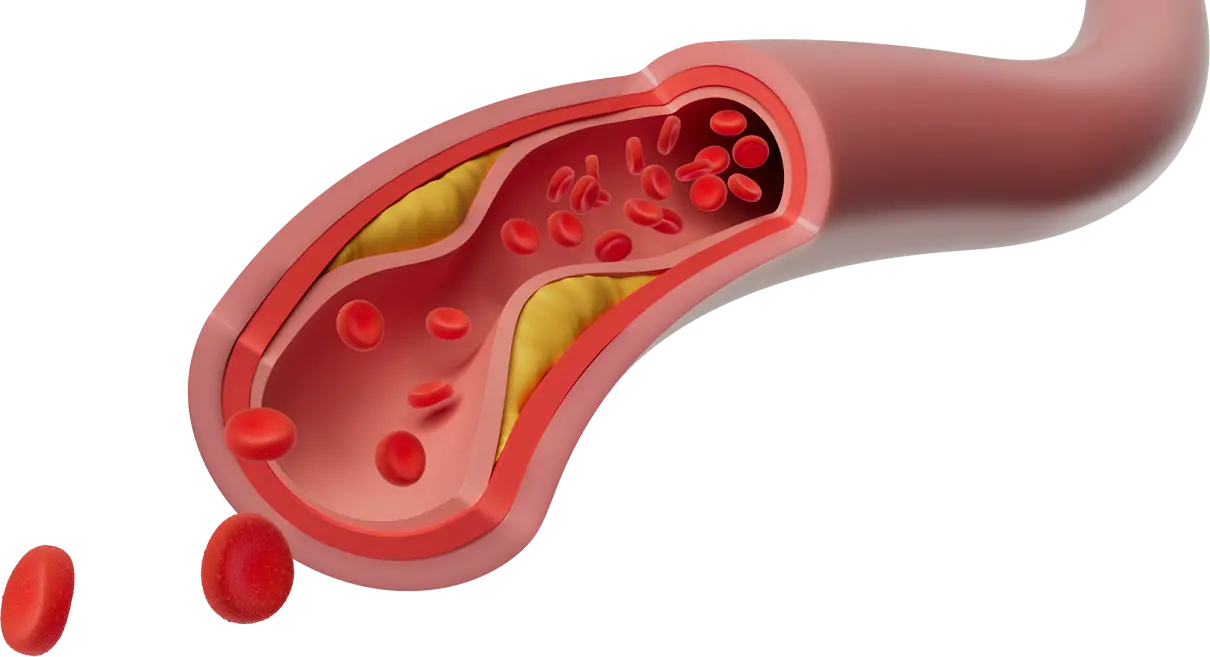
The initial trigger for the development of hardening of the arteries is probably damage to the endothelial cell layer lining the artery. This damage may be caused by smoking, viruses, chemicals and drugs. There may be many chemical causes of damage to the endothelial cells in our environment that have not been identified. In the earliest stages, yellow fatty streaks develop in the blood vessels caused by the deposition of fats in the wall of the artery. They are yellow due to the deposited cholesterol. Fatty streaks will not cause any symptoms, but are the earliest sign of arterial disease and can progress to the development of atherosclerotic plaques. Plaques are basically thickening of the innermost layer of the arterial wall. As the plaques become larger they impede blood flow through the artery.
Plaques are caused by the accumulation of low density lipoprotein (LDL, a type of cholesterol). Raised levels of LDL in the blood stream lead to the transport of this excess LDL into the artery wall where it is retained. This LDL is then chemically altered (lipid peroxidation) and as more is retained a massive accumulation of cholesterol develops (foam cells). Other cells (monocytes) are attracted towards this altered LDL by inflammatory chemical compounds and accelerate the accumulation of further LDL. A fibrous plaque develops as smooth muscle cells and monocytes accumulate. Monocytes are also prevented from leaving the early forming plaque by certain chemicals. The monocytes transform into another cell type called macrophages which absorb the cholesterol and fats deposited in the arterial wall. The macrophages become swollen with cholesterol and become foam cells (Gerstzen RE and Tager AM, 2012). The plaques can become so thick that they protrude into the artery and can interfere with normal blood flow.
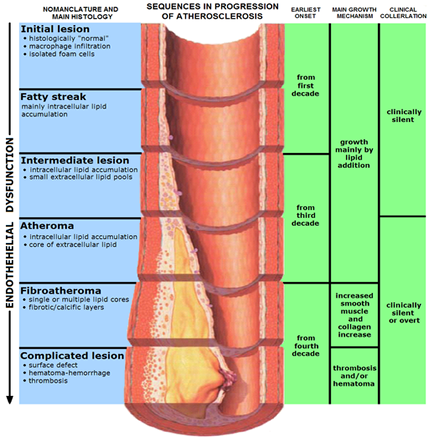 Complicated plaques develop if the plaque surface becomes damaged (ulceration) and this can cause fragments of the plaque to break away into the blood vessel and be carried downstream to block a smaller blood vessel – a process called embolisation. In more advanced cases calcium is also deposited and the plaques become very hard. These plaques may grow so large that they obstruct the flow of blood through the blood vessel or they may fracture and blood can be forced underneath the plaque, pushing it further into the blood vessel. When an artery becomes blocked by hardening of the arteries blood is diverted into smaller arteries (collaterals). These smaller arteries can maintain a blood supply to an area even when the main artery has been blocked.
Complicated plaques develop if the plaque surface becomes damaged (ulceration) and this can cause fragments of the plaque to break away into the blood vessel and be carried downstream to block a smaller blood vessel – a process called embolisation. In more advanced cases calcium is also deposited and the plaques become very hard. These plaques may grow so large that they obstruct the flow of blood through the blood vessel or they may fracture and blood can be forced underneath the plaque, pushing it further into the blood vessel. When an artery becomes blocked by hardening of the arteries blood is diverted into smaller arteries (collaterals). These smaller arteries can maintain a blood supply to an area even when the main artery has been blocked.
As the disease worsens the arteries literally become harder and lose their elasticity or stretchiness.
For a more detailed, but technical description of the mechanisms behind the development of atherosclerosis see JA Berliner et al, 1995
Why do some people develop hardening of the arteries?
There are many factors associated with hardening of the arteries, but there are only 4 or 5 which can be manipulated – smoking, high blood pressure, high cholesterol levels, presence of diabetes, and exercise.
In some people there is a clear hereditary factor. In other words other members of the family will have suffered with atherosclerosis at an early age. This may be due to risk factors that we have not yet discovered, but it can also be due to inherited diseases of cholesterol metabolism. If you are a man, you have more risk of developing hardening of the arteries.
It is often a combination of factors that is important. High blood pressure alone carries risks, but if there are high cholesterol levels also and a family history of atherosclerosis, the risks will be much greater.
In recent years certain types of infection (Chlamydia pneumoniae) have been implicated in atherosclerosis. No definitive link between infection and atherosclerosis has been established, but it is an area of ongoing research.
What problems can hardening of the arteries cause?
Hardening of the arteries causes two major types of problems in the arteries. Firstly, it may cause swelling /dilatation of the arteries to form aneurysms. Aneurysms can ultimately either rupture and bleed or they may accumulate large amounts of blood clot and either block or send showers of tiny clots into smaller arteries downstream (embolisation).
Secondly, hardening of the arteries causes the artery to narrow or block off completely. If an artery is narrowed or blocked then the effects of this will depend on which artery is affected. If the arteries to the legs are affected, then this can cause intermittent claudication – a pain in the legs on exercising.
If the arteries to the brain are affected then this can cause a stroke. If arteries to a part of the brain are blocked then this part of the brain dies. If this part of the brain controls movement of the right arm, then paralysis of the right arm will result.
If the arteries to the heart are affected this can cause angina (chest pain) or a heart attack. In the kidneys hardening of the arteries can cause kidney failure and high blood pressure (hypertension).
Can hardening of the arteries be cured?
No. Hardening of the arteries cannot be cured at present.
The symptoms that are caused by hardening of the arteries can sometimes be treated. For instance carotid endarterectomy is an operation to fix the damage caused by hardening of the carotid arteries in the neck. The carotid arteries take blood to the brain.
Angioplasty can be used in some circumstances to treat the symptoms caused by hardening of the arteries particularly in the arteries to the legs and to the heart. Angioplasty does not affect the underlying atherosclerotic processes – it is purely a mechanical method of re-opening the blood vessel. This point is often forgotten. Angioplasty and bypass surgery do not alter the development of atherosclerosis. This is a similar situation to calcium scale which can develop on kettles and pipes in areas which have hard water (containing calcium). The scale can be removed and allow the pipes to function again, but they will fur up again if the water is not altered, as the underlying cause has not been addressed. Coronary artery bypass surgery is used to improve the blood flow to the heart when patients have angina or have had a previous heart attack. Similar sorts of bypass surgery can be used to treat blockages in the legs.
The factors that lead to the development of hardening of the arteries can be altered. Controlling these vascular risk factors is important because it can help to reduce the risk of further problems caused by hardening of the arteries.
What can be done to reduce the risk of developing problems?
1. Smoking
Smoking is the most important factor. If you smoke and have problems with your arteries you should stop immediately. This can be difficult. Smoking is physically and mentally addictive. If you stop smoking you will not always feel the benefits immediately – it takes time. There are many ways in which you can be helped to stop smoking by your own general practitioner. These include nicotine patches, drugs and continuing support. The most important factor in quitting tobacco is actually wanting to stop. If you live in a house with another smoker it can be especially difficult to quit and a team effort is likely to be needed.
2. High blood pressure
If you have high blood pressure this should be treated as this reduces the risk of further arterial problems. Exercise and possibly dietary salt restriction may be helpful in maintaining a normal blood pressure. The individual benefits of treating blood pressure are of a similar order to treating cholesterol (see below).
3. Cholesterol
If your cholesterol level is high this should be lowered. A low fat diet can help, but you may need tablets to keep cholesterol levels low. Several beneficial effects of lipid lowering drugs may be due to their anti-inflammatory properties. Although lowering cholesterol levels is clearly helpful the potential benefits to any individual patient are actually very small. Exercise can also be helpful in lowering cholesterol levels.
A recent analysis of 14 trials involving over 90,000 patients has reported on the actual benefits from cholesterol lowering therapy (CTT Collaborators, 2005). The risk of dying can be reduced from 9.7% (9 to 10 chances in 100) over the periods studied down to 8.5% (8-9 chances in 100). Essentially this means that 98-99 people in every 100 people on a cholesterol lowering drug will not live longer, and the drug will not reduce their risk of dying. There are slightly greater reductions in risk of having heart attacks, but less benefits in terms of reduction of stroke risk. The same sort of benefit is seen with interventions such as for blood pressure lowering. When patients start these, frequently lifelong, medications it is often not made clear that the individual benefits are extremely small.
The Heart protection study examined the effect of simvastatin on reducing the risk of major vascular events (stroke, heart attack), but not mortality. There is more benefit in patients with peripheral vascular disease (PVD). There was a reduction in major vascular events in patients with PVD of 6.3% (from 32.7% to 26.4%). Definitely beneficial treatment but 93% of patients who use simvastatin in these circumstances will still have no benefit.
The CTT collaborators also examined the effect of cholesterol lowering treatment in patients with diabetes. The overall risk of death in patients with diabetes was reduced by taking cholesterol lowering treatment from 11.9% to 11.0%. A reduction of 0.9%. Less than 1 in 100 patients will live longer on this treatment. There was a greater reduction in any vascular event (stroke, heart attack or heart operation) from 19.2% to 15.6%. A reduction of 3.6%. Less than 4 patients in 100 will benefit.
Another way of looking at treatment is the number of tablets it would take to save one life. In the 4S (4S, 1994) trial of cholesterol reduction over 59,000 tablets would have to be taken to prevent one death. An interesting perspective on risk reduction can be found in this article published in the British Medical Journal.
4. Diabetes
If you have sugar diabetes (diabetes mellitus) this can be treated with insulin, tablets and sometimes diet alone to maintain a normal blood sugar. Diabetes has been known to cause hardening of the arteries for a long time. It can cause particularly severe calcium deposits in the blood vessels. Controlling diabetes with insulin, diet and tablets can reduce the chances of arterial disease developing or progressing, but here again the evidence from trials is that the benefit is relatively small.
5. Exercise
Regular exercise can help to lower cholesterol levels as well as improve exercise tolerance and general well being. It is generally recommended that exercise needs to take place for 20 minutes, 3 times week. The exercise needs to increase the heart rate to be beneficial. If you have not exercised for some time it is important to build up your exercise regime very gradually. It may take 6-8 weeks before you start to notice real benefits in fitness and wellbeing. A recent study from Australia indicated that watching TV can be detrimental to life expectancy and this effect is almost certainly mediated though the fact that prolonged hours watching television reduces exercise whilst food intake will continue whilst inactive..
6. Drugs
There are no specific drugs that will cure atherosclerosis, but taking a small dose of aspirin (75mgs) daily, if you have had previous problems with your arteries, can be helpful in preventing further problems. A recent overview summarised data from over 9000 patients in 42 trials and concluded that aspirin provided a relative risk reduction of 23% in the risk of cardiovascular events (stroke and heart attack) and cardiovascular death (Hackam DG, 2005). The absolute benefit is much smaller and in the range of 2% – 4%. This means that only between 2 and 4 people in every 100 taking aspirin will have any benefit. The other 96-98 out of every 100 who take the drug do not benefit.
Aspirin should be avoided if you have had previous problems with stomach ulcers or duodenal ulcers.
Clopidogrel is a more expensive alternative for patients intolerant of aspirin. It has no major advantages over aspirin and a recent study has not demonstrated any advantage when taken with aspirin (CHARISMA Investigators, 2006).
Dipyridamole, another antiplatelet drug, but working through a different mechanism to aspirin, has shown a small benefit if combined with aspirin when compared with aspirin alone (ESPRIT study group, 2006) but many more patients need to stop the combination due to side effects. It has been estimated that adding dipyridamole to aspirin would prevent about 10 extra vascular events per 1000 patients treated (Sudlow 2007). Alternatively 990 patients out of every 1000 taking dipyridamole in addition to aspirin would do so with no benefit.
Adding warfarin (another oral blood thinning drug) treatment to aspirin was also of no overall benefit over a 35 month follow up period and carried an increased risk in terms of life threatening bleeding (The warfarin antiplatelet vascular evaluation trial investigators, 2007).
Primary prevention
The treatments and benefits described above are examples of how patients can be treated when they have suffered a vascular event such as a heart attack or stroke or suffer with claudication pains in their legs. When they have established vascular disease and are being treated with preventive therapies this is described as secondary prevention. Primary prevention is treating patients for vascular risk factors before they develop vascular diseases. Unfortunately, although an attractive concept, primary prevention has even less (if any) benefits than secondary prevention. For instance in a study of aspirin 99.94% of patients would not benefit from treatment even though the effect of aspirin on the 0.06% of patients was shown to be highly statistically significant (ATT Collaboration).
In the West of Scotland cholesterol lowering study 200 men without any previous heart disease would have to swallow over 357,000tablets (yes, that’s correct) over five years to save one of them from dying from coronary heart disease
In other studies (Fowkes et al 2010, Belch et al 2008) patients were identified as having hardening of the arteries after measurement of their ankle-brachial index. These patients had no history of vascular disease and they were then randomised to treatment with aspirin or a sugar pill (placebo) to see if aspirin was beneficial in reducing the future risk of cardiovascular events. One trial also looked at the use of antioxidants (Vitamin C, zinc sulphate, sodium selenite, alpha tocopherol, pyridoxine hydrochloride, nicotinamide and lecithin). Despite being a large well conducted studies there was no benefit in taking aspirin or antiooxidants in patients without previous cardiovascular disease.
Latest news
An article (Wald and Law) in the British Medical Journal has suggested that producing a Polypill could reduce heart problems by 88%. The authors estimate that one third of patients taking this pill from age 55 would benefit, gaining on average 11 years of life free from heart problems or stroke. Because hardening of the arteries usually affects all arteries in the body to some degree, the Polypill strategy would be just as likely to reduce problems caused by hardening of the arteries in the legs.
The ingredients of the Polypill are drugs in common use today. They are:
- a statin (to lower cholesterol)
- a thiazide diuretic, a beta blocker and an angiotensin converting enzyme (ACE) inhibitor (to lower blood pressure)
- folic acid (to reduce homocysteine)
- aspirin (to reduce blood clotting)
At present this combination is only a suggestion and the formulation would need to be thoroughly tested. However, these drugs already have a proven track record. The recent Indian Polycap study examined the feasibility of using a “polypill”. The study looked at patients over a 12 week period and did find a reduction in blood pressure. No further benefits could be demonstrated in a short study. This proposal is being actively developed further and has potential, although the absolute benefits for any given individual are still likely to be small. In addition there is little incentive for the pharmaceutical industry to invest in studies as these medications are off patent.
Useful links
References
Berliner JA, Navab M, Fogelman AM et al. Atherosclerosis: basic mechanisms. Oxidation, inflammation and genetics. Circulation 1995; 91: 2488-2496.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. New Engl J Med 2005; 352: 1685-95.
Gerszten RE, Tager AM.The Monocyte in Atherosclerosis — Should I Stay or Should I Go Now? New Engl J Med 2012; 366: 1734-1736.
Wald NJ, Law MR. A strategy to reduce cardiovascular disease by more than 80%. Brit Med J 2003; 326: 1419-1423.
Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 2005; 366: 1267-78.
Heart Protection Study Collaborative Group. Randomized trial of the effects of cholesterol lowering with simvastatin on peripheral vascular and other major vascular outcomes in 20,536 people with peripheral arterial disease and other high risk conditions.J Vasc Surg 2007; 45: 645-54.
Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy of cholesterol-lowering therapy in 18686 people with diabetes in 14 randomised trials of statins: a meta analysis. Lancet 2008; 371: 117-125.
The Scandinavian Simvastatin Survival Study Group: randomised trial of cholesterol lowering in 4444 patients: the Scandinavian simvastatin survival study (4S). Lancet 1994; 344:1383-1389.
Hackam DG. Cardiovascular disease prevention in peripheral artery disease. J Vasc Surg 2005; 41: 1070-3.
ESPRIT study group. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPIRIT): randomised controlled trial. Lancet 2006; 367: 1665-73.
Sudlow C. Give dipyridamole with aspirin instead of aspirin alone to prevent vascular events after ischaemic stroke or TIA. Brit Med J 2007; 334: 901.
CHARISMA investigators. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 2006; 354: 1706-14.
The warfarin antiplatelet vascular evaluation trial investigators. Oral anticoagulant and antiplatelet therapy and peripheral arterial disease. New Engl J Med 2007; 357: 217-27.
Antithrombotic trialists collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009; 373: 1849-60.
Shepherd J, Cobbe M, Ford I, Isles CG, Lorimer AR, MacFarlane PW, et al for the West of Scotland Coronary Prevention Study Group. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. N Engl J Med 1995;333:1301-7.
Fowkes FGR, Price J, Stewart MCW. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index. A randomised controlled trial. JAMA 2010; 303(9): 841-848.
Belch J, MacCuish A, Campbell I et al. The prevention of progression of arterial disease and diabetes (POPADAD) trial: factorial randomised placebo controlled trial of aspirin and antioxidants in patients with diabetes and asymptomatic peripheral arterial disease. Brit Med J, 2008; 337: a1840.
Veerman JL, Healy GN, Cobiac LJ et al. Television viewing time and reduced life expectancy: a life table analysis. J Sports Med 2011: published online first.